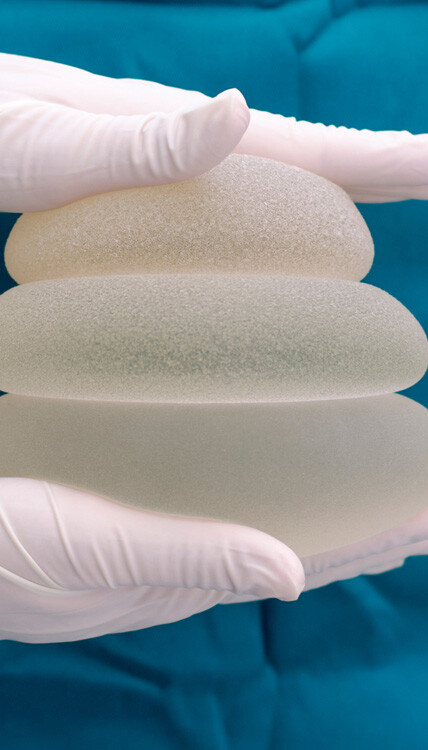
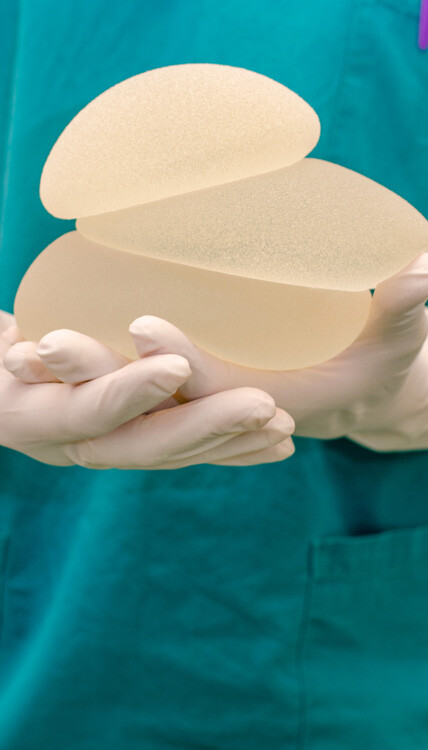
Breast augmentation is a surgical procedure to make breasts appear larger and fuller. Performed using either special implants or by fat transfer from a different area of the body, the procedure helps to restore breast fullness after pregnancy or weight loss, correct asymmetrical breasts, or enlarge smaller breasts. It is also valuable as reconstructive surgery after a mastectomy or other breast surgery.
A safe, effective procedure
When done by a skilled and experienced board-certified plastic surgeon, breast augmentation is a safe and effective procedure. The surgeon takes the necessary measures to minimize the risks of the operation, and the majority of women have no issues after the surgery. In fact, among millions of women with breast implants, complications have been observed in fewer than 1% of patients.
However, like every surgery, the procedure has general surgical risks, including temporary pain, swelling, bruising, tightness in the chest, bleeding, infection, poor scarring, allergic reaction to anesthesia, hematoma, changes in breast or nipple sensation, or need for revision surgery.
Besides, breast implants are designed to be temporary devices which wear out, degrade chemically, and release their content. So when getting breast implants, women should know that they are temporary devices that will need removing or replacing at a later date—the longer you have the implants, the higher the chances of complications.
What are the specific risks and complications of breast augmentation?
1. Pain
You will experience some pain or contraction for a while after the operation. Your surgeon can prescribe pain-relieving medication to help you manage pain which should be gone after 7-10 days. Do not take any other medication apart from the painkillers and additional medications prescribed by your doctor.
2. Seroma
Seroma — a buildup of fluid under the skin surface—may occur after the procedure, often at the site of the incision. The fluid is called serum and may begin to accumulate soon after surgery or several weeks later. Seromas pose a risk of infection and are resolved by draining the fluid buildup, especially when they are large.
3. Breast Implant-Associated Illness
Breast implant illness (BII or BIAI) is a self-reported complication and not an official medical diagnosis. Patients who believe they have the condition have reported a number of common symptoms, including fatigue, chest pain, hair loss, chills, headaches, chronic pain, rash, anxiety, photosensitivity, brain fog, and sleep disturbance.
There is still a need for research to find out why the symptoms occur and how they can be remedied. Many patients reporting these symptoms have also reported that the removal of breast implants alleviates the symptoms.
4. Implant rupture and deflation
Although breast implants have changed significantly since their inception and are now more durable than before, they can still rupture or burst under trauma or extra pressure. Most implant ruptures occur between 10-15 years after initial surgery, but this depends on the type of implant.
Silicone gel-filled implants have thicker liquid, so they do not deflate completely after rupture. But a hole or tear in saline-filled implants can cause a complete deflation, as the fluid escapes into the surrounding tissue.
Silicone implant rupture comes with risks such as pain, lumps, tenderness, and swelling. The breasts are also deflated in a manner visible to the eyes. Therefore, for patients with silicone gel-filled implants, it is advisable to have regular MRI scans after the procedure to detect possible rupture. If rupture is found, the implants are removed and replaced to prevent infections, discomfort, and cosmetic deformities.
5. Capsular contracture
The natural tissue of the body may react to the breast implants through an immune response. When this occurs, the collagen fiber around the implant forms a scar tissue (membrane) around the implant, resulting in hardening, stiffness, implant deformity, and pain in the breast over time.
Capsular contracture is classified into four grades: I to IV. Grade I contracture can go away with massaging and usually does not need treatment as it causes minimal problems. Grade II contracture creates more firmness in the breast and requires ultrasonic massage instruments. Grade III and IV contracture makes the breast hard and unnatural and requires surgery to remove and replace the implant.
6. Hypertrophic scarring
Breast augmentation is associated with a severe form of scarring, called hypertrophic scarring. It is a small but notable risk—only observed in 5% of patients. It is characterized by a thick, red-colored scar that is raised above the skin. Surgical scars tend to occur around the nipple and the lower part of the nipple. Your plastic surgeon may carry out renovation procedures to eliminate or reduce these scars.
7. Breast Implant-Associated Anaplastic Large-Cell Lymphoma
Though there is a low risk of Breast Implant-Associated Anaplastic Large-Cell Lymphoma (BIA-ALCL) occurring after breast augmentation, patients should still be aware of the risk. BIA-ALCL is a cancer of the immune system and is not related to breast cancer.
The condition is curable, with early detection offering patients the best chance for a quick recovery. Women considering breast augmentation should speak with their plastic surgeons about the risk of BIA-ALCL.
8. Surgical site infections
Infection may develop in or around the surgical site if bacteria enter the surgical wound either from the skin or in a contaminated saline solution or implant. The infection may be mild or severe, with the potential of infiltrating into deeper layers of the skin. Symptoms include pain in the surgical area and high fever. The implant may need to be removed to allow for the treatment of the infection before it is eventually replaced.
At Politis Plastic Surgery, we understand that the possible risks and complications of breast augmentation vary depending on your medical history, body type, allergies, medication, and other individual factors. We uphold the highest standards of medical care and take the necessary steps during the procedure to minimize the risks associated with the surgery. And after the procedure, we will keep in touch with you to ensure that any issues are promptly resolved.
Want to meet with a plastic surgeon to have your specific questions and concerns addressed? Dr. Effie Politis will listen to your cosmetic goals, explain available options, and guide you through your preparation for the surgery and your post-surgical journey. For more information on breast augmentation, visit the site Politis Plastic Surgery website.