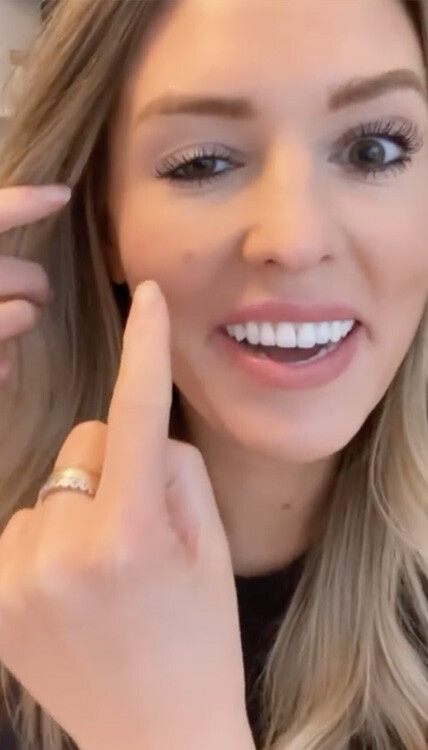
Last April, Chicago-based influencer and blogger, Whitney Buha, shared about an unfortunate experience with a cosmetic procedure gone wrong.
What exactly happened and what can be done about it?
I shared my thoughts about it in this quick video.
Also, I talked a little bit of what I do with regards to using Botox in my own practice.
What do you think about this incident? As a fellow plastic surgeon, as a patient, or as someone who is considering this procedure?
Why do women undergo breast explantation?
Hi everyone it’s Dr. Effie Politis and I’d like to talk about a great article on the April edition of the PRS called
“Contemporary Strategies in Breast Explantation Surgery”. So what is explantation surgery? It is a surgery in which someone proceeds with removing their implants and not replacing them. I’m seeing quite a few patients that are interested in the surgery for various reasons. We all know that implants are man-made devices.
The first reason that women would opt to undergo the surgery is because of implant rupture.
I tell women that breast implants are not a one and done device. They are prosthetics that are placed in your body, so you need surveillance and you likely will need one or several surgeries in the future if you opt for breast implants. There is a small chance of them rupturing, we can discuss more on the differences between saline and silicone ruptures in the future.
Is breast implant associated with ALCL
This is a rare lymphoma associated with texture implants, which I do not use, so it’s not really an issue with my practice but I do see patients with prior history of textured implants.
Is breast implant illness?
This is a large topic that’s often discussed on social media. It’s the name given to patients for a wide range of symptoms. The current data shows there’s no cause and effect relationship between implants and the symptoms. However we certainly are proponents of what women want to do with their body, so if they want their implant removed they certainly have the right to have that done. However, the data based on long term studies does not show whether explantation surgery reliably reduces these symptoms.
The last reason why women want their implants removed is for non-medical reasons, like the effects of aging, weight changes, pregnancy and shifting perspectives in aesthetic beauty.
As we know there is a movement towards a smaller breast. So women seeking explantation surgery just need to be aware of the risk and benefits and any adjunct surgeries that can be done to enhance their breast. We look at each woman on an individual basis. It’s a woman’s choice to have her implants removed and we consider the patient’s risk profile, patient preference as well as safety when guiding them on whether explantation surgery is the right surgery for them. I would advise you all to always consult with a board-certified plastic surgeon with a specialty in breast surgery when considering these types of procedures. You can always DM me or look at my website, I’ll have more information. Thank you so much
Lip Restoration and Shaping
On achieving lower facial optimization
This patient displays typical age-appropriate changes in lips: maxillary retrusion leading to lack of bony support, elongation of upper lip unit, loss of philtral definition, architectural changes (loss of fascia/ligamentous support), deflation of the vermillion, as well as dynamic peri-oral rhytids.
I typically have patients animate and evaluate them while talking. I also evaluate their lip tooth ratio while in repose and while smiling.
I evaluate the chin and mentalis muscle as well as mandibular support. The correct analysis helps me make recommendations for surgical correction versus volumetric enhancement. This patient passed my criteria for volumetric enhancement with filler to restore youthful contours and ratios.
This patient received only I cc Revanesse Versa lip filler. I like this filler because it is prehydrated, meaning, less swelling and a softer appearance. I also like RHA2 in lips and Restylane Kysse for my younger patients. If I need more border definition I often go to a Restylane Refyne or Defyne. Sometimes I combine fillers to optimize different rheologic properties.
I massage lips and apply moisturizer.
Expect bruising and swelling to subside at 5-7 days.
More to come on surgical correction or lip lift
Renuva a Great Alternative to Autologous Fat Transfer
Renuva is great alternative to autologous #fattransfer and #facial-rejuvenation . Given the well documented fat loss starting in our late 30’s and accelerated in the 40’s and 50’s… this is a good volumizer that recruits your own fat cells into a honeycomb lattice that lasts! Your own fat is recruited over 3 months to replace the shelf fat in syringe. No downtime and great for those with #fillerfatigue or those wanted a more lasting, natural look. What’s better than recruiting your bodies own fat? Call or DM our office for more info!
What Is The Fat Transfer Procedure?
Autologous fat grafting, or fat transfer, is a procedure that allows your surgeon to transfer your own fat from one area of your body to another.
Fat transfer is often used for aesthetic and reconstruction procedures to:
• Enhance volume and fullness of body areas with soft tissue loss or deficiency
• Contour or reshape body areas
• Improve overall symmetry and fine-tune body proportions
In fat grafting, fat tissue is removed from other parts of your body — usually your thighs, belly, and buttocks — by liposuction. The tissue is then processed into liquid and injected into the breast area to recreate the breast.
REVOLVE™ System is designed to remove localized deposits of excess fat through small incision and subsequently transfer the tissue back to the patient. Use of this device is limited to those physicians who, by means of formal professional training or sanctioned continuing medical education (including supervised operative experience), have attained proficiency in suction lipoplasty and tissue transfer. (source: revolvefatgrafting.com)
If you want to know more, ask a #boardcertifiedplasticsurgeon for a FULL-BODY CONSULTATION to discuss the benefits of fat transfer.
What is PRF Treatment?
PRF is now one of the most highly sought out cosmetic non-surgical procedures.
It is an all-natural solution that can treat areas in the face that show the first signs of aging, like under-eye hollows, deflated cheeks, and scalp for hair restoration.
This has platelets, fibrin, and white blood cells, which help achieve wound healing, collagen production, and improved overall elasticity.
As for its benefits, I will talk about it more in a future post!
Stay tuned!
And if you have some questions, comment them down below, and we will address them in our next post!
If you are interested in this procedure,
Call us: (813) 542 – 2587
Check our website: politisplasticsurgery.com
Visit us: 5016 West Cypress Street, Suite 200, Tampa, FL 33607
What Are The Signs You Have Capsular Contracture?
Capsular contracture develops in one or both breasts and can occur at any time, either in the weeks following breast implant surgery (this occurs most often) or, in some cases, years later. Its signs and symptoms often develop gradually over time, making it difficult to identify the complication early if you aren’t sure what you are looking for.
Early signs of capsular contracture may include a firm or tight sensation, pain, or asymmetry.
As the condition worsens, you may notice more obvious symptoms, including:
- Breast pain
- Asymmetry
- Firmness
- Tightness
- Round or ball-shaped breast
- High-riding breast
- Misshapen breast
If you start to notice any signs that you suspect are associated with capsular contracture or another breast implant complication, call your surgeon right away to be evaluated and learn your options.
Before and After Look with Refresher Facelift
This lovely patient flew in for a total refresh in office. She underwent mini facelift with SMAS plication to rejuvenate mid face, as well as myomodulation with toxin/filler combo to optimize structural support and minimize dynamic lines of expression.
Monday Mommy Makeover
Monday Mommy Makeover!
Motherhood brings joy, but it can also take a toll on your body. In fact, pregnancy can cause unwelcomed changes that include a stubborn tummy, sagging breasts, noticeable stretch marks, or persistent pockets of fat around the thighs, arms, and waist.
While you can often reverse these changes through lifestyle modifications like better nutrition and exercise, in some cases the changes seem stubbornly resistant to improvement, and it can be quite frustrating to feel that you have to live with them for a long time.
Enter, the mommy makeover.
At Politis Plastic Surgery, we see many women who simply want to look the way they did before they had children, and we are happy to recommend mommy makeover surgeries.
Here’s one of our patients who had undergone the mommy makeover procedure!
Is mommy makeover right for you?
We provided more information on our website. You can access it through the link in our bio.
Facial Treatment Guide: What Are My Options?
Here is a facial treatment guide with the options that you can avail in Politis Plastic Surgery.
A lot of the areas shown in the diagram can be treated with fillers. I use a wide range of fillers for different reasons. I have put HA filler to reflect hyaluronic acid-based fillers.
I use a variety of fillers, including the Restylane products, Juvederm Rep products, and a newer one called RHA1/2/3 made by Teosyal. I am using Radiesse more than sculptors as my biostimulator of choice.
I use Kybella to remove/treat submental fat, and also jowl fat, as well as other areas of the body with excess fat.
In addition, I’ve added neurotoxins to a lot of areas. I like to use neurotoxins in conjunction with a filler for myomodulation. This is a multi-modal approach to relax the vector of pull on the muscle which then can help optimize facial shaping with the fillers.
I also want to note that the RHA filler line is known for a layering effect. This means that the rheology or physics behind the fillers allow them to be layered on top of each other for optimal facial shaping. We also use Versa filler quite a bit for lips augmentation, chin, and nose-shaping.
Again, here are the products mentioned above:
FILLERS:
NEUROTOXINS: (General term for Botox which is a brand)
- Jeaveau
- Xeomin